There is no need to believe in conspiracy theories to explain the current explosion of infectious pandemics.
Here is the explanation (I hope that my audience can assist laymen to understand what follows through the creation of charts and/or rephrasing of statements):
Use of vaccines in the absence of the circulating target pathogen will not allow an individual or even an entire population to exert suboptimal immune pressure on the pathogen’s life cycle
However, as soon as the pathogen is circulating in a population, it becomes possible to put suboptimal immune pressure on its life cycle
If suboptimal immune pressure is only exerted by a small subset of the population, it doesn’t pose a major problem (however, this may already suffice for ‘seasonal’ vaccines, for example, to become less and less useful; example: seasonal Flu vaccines)
However, if suboptimal immune pressure is exerted by large parts of the population while the pathogen/ virus is circulating, then it becomes worrisome
Suboptimal population-level immune pressure becomes even more worrisome when thecirculating virus is a viral variant (i.e., different from the viral lineage that originally primed the population). This will drive natural selection of more infectious immune escape variants that will eventually adapt to the population because they’ve gained a competitive replication advantage. When that happens, the variant becomes dominant. Of course, increased viral infection rates will result in increased progeny of mutants; this will expedite the selection of appropriate variant(s) to overcome the suboptimal immune pressure exerted on their life cycle. When ‘more infectious’ variants begin to dominate, the likelihood for previously asymptomatically infected people to become re-exposed will augment. As a result of previous asymptomatic infection some of them may have developed short-lived titers of antigen(Ag)-specific, non-neutralizing antibodies (Abs). Non-neutralizing Abs can, however, enhance viral infectiousness if they bind in sufficient quantities to the virus (so-called Ab-dependent enhancement of infection; ADEI). However, the chance for a re-infection to occur shortly after primary infection is normally low unless the virus is very infectious or highly concentrated, or the cell-based innate immune system (CBIIS) is weakened (worst case scenario exists in densely populated areas with poor hygiene conditions and inadequate nutrition). In case ADEI occurs, the infection rate in the population will increase. This makes it now more likely for the virus to break through the cellular innate immune defense and trigger the adaptive immune system. Due to ‘antigenic sin’, adaptive immune triggering will, however, first recall the ‘old’ Ag-specific Abs (i.e., those that were acquired as a result of the original immune priming). Although these antibodies will be recalled rapidly and in large quantities (because of immunologic memory!), they will not do well at recognizing the dominantly circulating ‘more infectious’ variant. Consequently, the neutralizing capacity of these Abs will diminish. This increasingly enables non-neutralizing Abs to bind to the virus, and thereby promotes an even more pronounced ADEI effect. The more infectious the dominant variant becomes, the more strongly and frequently the virus will break through the host’s innate immune defense. Simultaneously, titers of antigen(Ag)-specific Abs will continue to rise and their neutralizing capacity continue to diminish. This will result in an increased likelihood for ADEI to occur and a higher susceptibility of the population to re-infection.
The phenomenon described above does not normally occur during natural infection with glycosylated viruses causing acute self-limiting viral infection (ASLVI)—this is because these viruses are largely eliminated by cell-based innate immunity (e.g., NK cells). Unless the virus is very infectious or highly concentrated or the CBII weakened, innate immune effector cells will be able to eliminate most of the virus before Ag-specific Abs begin to peak. This not only reduces the chance for these Abs to exert pressure on the viral life cycle (and hence, to contribute to immune escape) but also lowers the likelihood for potentially recalled Ag-specific Abs to bind substantial amounts of poorly matched viral variants upon re-exposure (all of which would see their replication more effectively[1] controlled by NK cell-mediated killing of the host cells they infect). This would, therefore, dramatically reduce the risk of ADEI and the impact on viral infectiousness would be low or even absent.
However, when non-replicating vaccines are used to induce an immune response to the virus, the cell-based innate immune system is bypassed and doesn’t get trained. Consequently, there is no mechanism to remove the bulk of the viral load before Abs can reach high titers of fully functional (i.e., neutralizing) Abs. When this occurs in a sufficiently large part of the population, natural selection and expansion in prevalence of more infectious immune escape variants will readily occur. Additionally, vaccine-primed individuals will generate much higher Ag-specific titers upon re-exposure and their Abs will not be a good match for a virus that previously escaped massive immune pressure (the latter can, indeed, only happen provided selection of an antigenically shifted variant that makes the virus sufficiently more infectious). The combination of a higher level of intrinsic viral infectiousness with high titers of vaccinal Abs makes vaccinees much more prone to ADEI. ADEI will lead to a higher infection rate in the population and thereby more frequently boost previously primed Ag-specific Abs, thereby having a snowball effect and leaving vaccinees increasingly susceptible to ADEI.
However, in case of ASLVIs caused by glycosylated viruses, infection-enhancing Abs still prevent severe viral disease in distant organs (whereas the infection-enhancing Abs promote viral infection & replication in the upper respiratory tract by virtue of their virulence-neutralizing effect[2]). This typically generates a reservoir of asymptomatic shedders—they abrogate productive infection and prevent severe disease thanks to elimination of virus-infected cells by cytotoxic CD8+ T cells[3] . The cytolytic capacity of these cytotoxic T cells (CTLs) is fueled by infection-enhancing Abs that prevent transinfection in distant organs). This explains why these Abs are having a virulence-neutralizing effect[4].
Consequently, vaccinees pave the way for pandemics of viruses they asymptomatically shed/ transmit. By preventing trans infection, virulence-neutralizing Abs increase viral uptake by antigen-presenting cells (APCs) and thereby enable activation of poorly MHC class I-restricted CD8+ T cells that will not only kill host cells infected by the virus that is responsible for initiation of this cascade of immune events, but also host cells infected by other immunogenically related viruses (i.e., presenting the same CTL epitope on cell surface-expressed MHC class I molecules upon their internalization into APCs: e.g., common cold CoV, influenza virus, poxvirus, RSV).
However, the immune pressure exerted on viral virulence is only suboptimal as it cannot prevent productive infection. Nature will, therefore, proceed with natural selection and adaptation of viral immune escape variants that can overcome this immune pressure (see fig. 1; the molecular details of the SC-2 immune escape variants that I predict to be selected are described in)
Based on all the above, you should not fall into the trap of getting yourself vaccinated against monkeypox, avian flu or even seasonal flu virus with non-replicating vaccines
Health officials are now recommending vaccination against monkeypox using non-replicating vaccinia virus. However, usage of a non-replicating cowpox virus will only induce high titers of Abs that will not optimally recognize the circulating monkeypox virus. Although there is a high level of sequence homology among the surface proteins from cowpox, smallpox and monkeypox, it has already been established that the circulating monkeypox virus is rapidly evolving and adapting to the human population. In other words, high vaccinal Ab titers would already be confronted with a variant that the cowpox-matched Abs would not optimally recognize. This raises a serious concern in regard to Ab-dependent enhancement of disease (ADED), especially in unvaccinated people (i.e., who don’t ‘benefit’ from highly activated cytotoxic CD8+ T cells) with declining immunity (e.g., elderly, vulnerable people). The same applies, of course, to avian influenza virus which cannot be recognized by Abs induced or recalled by non-replicating influenza virus vaccines. On the other hand, live attenuated smallpox (or even influenza) vaccines are unlikely to work in healthy unvaccinated people with a thoroughly ’SC-2-trained’[5] innate immune system for lack of ‘vaccine take’ (though they would do no harm). Additionally, they would not be recommended for individuals with a weak innate immune system (elderly, vulnerable) for risk of causing severe disease.
However, the issue of ADED is currently not limited to zoonotic infections, but even to vaccine-derived poliovirus that has already been found spreading in countries that have high polio vaccine coverage rates. Fully immunized populations used to be protected against infection with poliovirus—however, the disruption of the polio vaccination program during the Covid-19 crisis combined with the enhanced circulation of vaccine-derived poliovirus (VDPV) after the WHO had withdrawn the oral type 2 vaccine around the world (2016) generated the ideal environment for the virus to escape from population-level immune pressure. Mass vaccination in third-world countries using a new OPV-2 vaccine that has a better safety profile (i.e., unlikely to revert to virulence) still induces Abs that are directed at the original polio type 2 strain (and not at the circulating variant, i.e., the VDPV) and is, therefore, only going to intensify immune escape even though the vaccine is live attenuated (that doesn’t help since ‘The horse has already left the barn’!). This is now leading to the dominant circulation of a poliovirus immune escape variant that can be expected to progressively increase its invasiveness/ infectiousness (so it will soon lose its ‘attenuated’ behavior), especially in populations that are highly vaccinated with non-replicating poliovirus! These populations will no longer be able to prevent infection whereas they will still be able to prevent disease (poliomyelitis). This will generate large cohorts of asymptomatic shedders (i.e., vaccinees) who are likely to ignite a new poliovirus pandemic. As immune escape is intrinsically correlated with ADEI, highly vaccinated populations in industrialized countries are likely to see a substantial increase in cases of ADEI-mediated poliomyelitis, especially in industrialized countries (see fig. 1).
Whereas trained innate immunity in people who experienced a productive SC-2 infection will largely protect them against diseases caused by other glycosylated viruses generating ASLVI, this does not apply to poliovirus (a non-enveloped, non-glycosylated virus). In my opinion, a poliovirus pandemic can only be prevented by the combination of improved water sanitation (potable water), environmental hygiene (e.g., no irrigation of food crops with wastewater), and, more importantly in highly vaccinated countries, by subcutaneous (instead of mucosal/ oral) administration of live attenuated poliovirus to prevent spread of VDPV (which, from the very beginning, has prevented eradication of poliovirus).
C-19 mass vaccination has transformed the globe in a breeding ground for more and more infectious pandemics
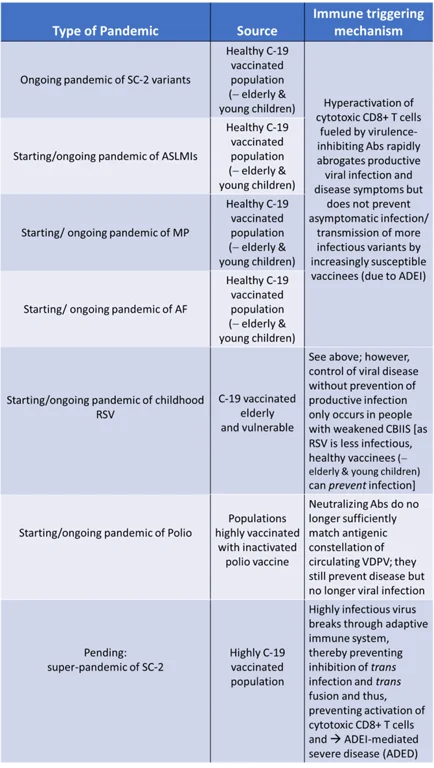
The list of starting/ ongoing pandemics is only growing (see fig. 2). The impact of these pandemics on individual, global and animal health has already been discussed.
Although all these pandemics will primarily generate disease in unvaccinated (parts of the) population(s) [see fig. 1], the latter should not be vaccinated because vaccination, especially with non-replicating viral vaccines, will only enhance immune escape and increase the likelihood for vaccinated individuals to contract ADEI or even ADED.
Fig.1:
Fig. 2:
ASLMI: Acute self-limiting microbial infection; VDPV: Vaccine-derived poliovirus
CBIIS: Cell-based innate immune system
[1] Upon re-exposure, NK cells will have been trained to more efficiently kill virus-infected cells and hence, reduce viral load. That’s why the Ag-specific Abs will no longer be able to bind large amounts of viruses
[2] https://www.voiceforscienceandsolidarity.org/scientific-blog/predictions-gvb-on-evolution-c-19-pandemic
[3] Those have no memory!
[4] https://www.voiceforscienceandsolidarity.org/scientific-blog/predictions-gvb-on-evolution-c-19-pandemic
[5] Because virus-associated self-mimicking peptides expressed on virus-infected cells at an early stage of infection are recognized by NK cells and shared among CoV and several other viruses (e.g., poxviruses and influenza viruses): G. Vanden Bossche; personal communication
This article was originally published on TrialSite News






"Use of vaccines in the absence of the circulating target pathogen will not allow an individual or even an entire population to exert suboptimal immune pressure on the pathogen’s life cycle
However, as soon as the pathogen is circulating in a population, it becomes possible to put suboptimal immune pressure on its life cycle"
Please clarify: You said to not vaccinate into a pandemic. Now you say to not vaccinate before a pandemic. Maybe your point is implied? Only vaccinate when the pathogen is circulating in low volume? If so, that is a really small window of opportunity. Much more needs to be said about this.
"Use of vaccines in the absence of the circulating target pathogen will not allow an individual or even an entire population to exert suboptimal immune pressure on the pathogen’s life cycle
However, as soon as the pathogen is circulating in a population, it becomes possible to put suboptimal immune pressure on its life cycle"
Please clarify: You said to not vaccinate into a pandemic. Now you say to not vaccinate before a pandemic. Maybe your point is implied? Only vaccinate when the pathogen is circulating in low volume? If so, that is a really small window of opportunity. Much more needs to be said about this.